Health Spending
Do countries get what they pay for when it comes to health care?
Key Messages
- Richer countries generally spend more on health care. But that doesn’t necessarily translate into better health outcomes.
- The U.S. has the highest health spending per capita among peer countries, yet it fares poorly on life expectancy, infant mortality, and premature mortality.
- Physicians in the U.S. are among the highest paid, but they are also most likely to have to pay the highest insurance premiums.
Why are we interested in health expenditures?
There is a general perception that “you get what you pay for.” But is it really true in health care? Does higher spending guarantee better health outcomes? The proportion of health-care spending in most industrialized countries is rising and, with aging populations, is expected to keep rising. Canada spent an estimated $191.6 billion on health care in 2010—up $9.5 billion from the previous year.1 Are Canada and its peers getting what they paid for?
Which country spends the most on health care?
The U.S. is by far the biggest spender when it comes to health—over US$7,500 per person in 2008. This is 50 per cent more than the second highest spender in the OECD, Norway. The U.S. also spends the largest share of GDP on health—16 per cent, which is five percentage points higher than second-place France. Canada spends 10 per cent of its GDP on health spending, or US$4,079 (at purchasing power parity) per capita.2 The U.S. also has the highest proportion of private expenditures on health and is the only country among its peers with a greater share of private than public spending.
Do richer countries spend more on health care?
In general, the richer the country, the greater the amount spent on health care. The chart plots the relationship between income and health spending for Canada and its peers. The trend line estimated from the data points shows a positive relationship: as income per capita increases, the amount spent on health care increases. Of course, there are variations among countries in the same income bracket. For example, in 2008, Canada, Australia, Denmark, and Finland had comparable incomes per capita, yet Canada spent much more per capita on health than the other three countries (US$4,079 per capita versus US$3,353 in Australia, US$3,540 in Denmark, and US$3,008 in Finland3). The U.S. is a big outlier; its health-care spending not only far exceeds that of other countries, it is also well above what one would expect for a country with its income level.
Do countries that spend more have better health outcomes?
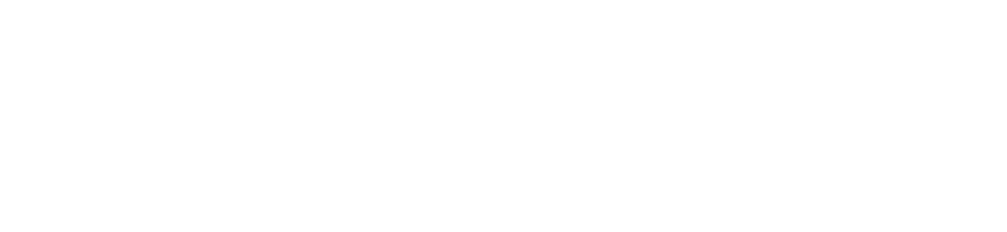
Apparently not—particularly when you examine life expectancy, which is a good overall measure of health outcomes. The U.S. actually has the lowest life expectancy among the peer countries. Interestingly, Japan, which has the lowest health-care expenditures per capita, boasts the highest life expectancy. Italy, which has the second lowest health spending per capita, has the third highest life expectancy among the peer countries. Norway has a higher income per capita than the U.S. and spends far less on health, yet its population has a much higher life expectancy.
On other key health outcomes such as infant mortality and potential years of life lost, the U.S. does equally poorly, ranking last on both. Conversely, Japan has the lowest expenditures per capita yet has the second lowest infant mortality rate (tied with Finland) and ranks among the lowest in potential years of life lost (after Sweden and the Netherlands). Meanwhile, Canada spends more on health care than Australia—a country with a comparable income per capita—yet the life expectancy in Australia is higher, and both infant mortality and the number of potential years of life lost are lower.
It’s easy to conclude that all this spending does not have much of an impact on health outcomes—particularly in the United States. However, many factors affect the health of a population—and where the money is being spent is just as important as how much is being spent.
Where is the U.S. spending its health dollars?
The largest proportion of health spending in the U.S. is on outpatient care. Outpatient care is medical treatment that does not require patients be admitted to a hospital or other medical facility for overnight stay. Outpatient care expenditures include basic medical and diagnostic services, specialized health care, and dental services. Relative to the peer countries, the U.S. spends the highest per capita on outpatient care.4 In 2008, the U.S. spent over $3,000 per capita on outpatient care—over two and half times more than the amount spent by the second highest spender, Sweden, and over three times the amount spent by Canada.
The U.S. has shifted much of its health-care services from inpatient to outpatient settings. One might expect that, as a result of this shift, total costs would decrease, given the higher costs associated with hospital stays. Not so. Any cost savings that might have been realized thanks to a decrease in hospital admissions have been more than offset by an increase in the number of medical visits, diagnostic exams, and day surgeries being performed. The lack of electronic health records is also an issue in outpatient care, particularly in a system with multiple competing insurance and health systems, because, as a result, tests and procedures are often duplicated. According to the Commonwealth Fund’s 2009 survey of primary health-care physicians, only 46 per cent of U.S. physicians surveyed reported using electronic patient medical records. In contrast, over 90 per cent of physicians surveyed in Australia, Italy, Netherlands, Norway, Sweden, and the U.K. use them.5
Outpatient care is more convenient for patients. The greater availability of services, coupled with the small out-of-pocket expenses, encourages many patients to take advantage of these services. Also, given that outpatient care is provided on a fee-for-service basis, health-care providers have an incentive to provide more health services. Specialists in the U.S. provide the largest proportion of primary care services, unlike in Canada and other OECD countries, where primary health care is primarily delivered by general practitioners, the “gatekeepers” of the health-care system. Specialists, however, have been shown to spend more than general practitioners.6 Outpatient care—such as specialist care and diagnostic procedures—is very profitable, and reimbursement methods for outpatient services encourage health-care providers to deliver more services.7
The increasing number of ambulatory surgery centres and diagnostic imaging centres, which give patients alternative options for immediate health-care services, are also driving up outpatient spending in the United States. Between 2000 and 2006, the number of ambulatory surgery centres grew by almost 8 per cent, and their market revenue grew by 13 per cent.8
A large proportion of same-day hospital care spending is on emergency room visits. According to McKinsey and Company, visits to the emergency department account for “$75 billion in annual costs and up to 56 per cent of total outpatient visits.”9 The frequenting of the ER is a reflection of poor access to primary health care.
Although inpatient care represents a smaller proportion of health-care spending in the U.S. than in other countries, the actual amount spent per capita is greater than that of its peers—only Norway spends more per capita on inpatient care.10 The high number of surgical procedures performed in the U.S. is one contributing factor to both its high inpatient and outpatient health-care expenditures. In the U.S., in 2006, 92.8 inpatient surgical procedures were performed for every 1,000 people—more than double the number in Canada (44.4 in 2007).11 Among OECD countries, the U.S. has the second highest number of knee replacement surgeries per 100,000 population, and the fourth highest number of caesarean sections per 100 live births.12 The U.S. also ranks high when it comes to surgical procedures related to heart disease, such as cardiac catheterization, coronary stenting, and coronary bypass surgery. In 2006, the U.S. had the third highest number of coronary bypass surgeries performed per 100,000 population, after Belgium and Germany.
Relative to its peers, U.S. health expenditures related to prevention are also high—only Canada spends more per capita on prevention and public health services.
The U.S. spends the most per capita in the OECD on administration and insurance health expenditures—over twice as much as the second highest spender in this category, France. This is not surprising given that the U.S. has a complex insurance model with high malpractice litigation costs.13
Do countries that spend more on health have more doctors and resources such as hospital beds and diagnostic equipment?
Not really. Key health resource indicators include the number of doctors and the number of hospital beds available. Despite all its spending, the U.S. ranks poorly on both indicators relative to its peers. There are only 2.43 practising physicians for every 1,000 people in the U.S.—well below the peer country average of 3.25 physicians for every 1,000 people.14 Both Canada and the U.S. also rank well below their peers on the availability of hospital beds. The peer country average for the number of hospital beds for every 1,000 people is 5.6—Canada has only 3.5 beds and the U.S. has only 3.1 beds.
When it comes to technologically advanced diagnostic equipment, such as magnetic resonance image (MRI) units and computer tomography (CT) scanners, Japan leads other countries by a significant margin, even though it also has the lowest health expenditures per capita. MRI equipment, however, costs much less in Japan than it does in other countries.15 At the opposite end of the spectrum is Canada, which ranks low on both the availability of CT scanners and MRI equipment. Although Australia has a similar income per capita to Canada, it spends a smaller share on health care, yet it has a higher proportion of hospital beds and CT scanners.
The U.S. ranks second, after Japan, on the availability of MRI units and third on CT scanners. Not surprisingly, the U.S. also ranks well ahead of other OECD countries on the number of diagnostic tests performed using this equipment. For example, in 2007, 91 MRI exams per million population were performed in the United States—over twice the OECD average.16 MRI and CT equipment is extremely expensive—the average MRI machine costs over $1 million—and exams performed with this equipment are costly. Medical liability and defensive medicine17 are one reason for the increased number of diagnostic exams in the United States. A study published in the journal Health Affairs attributes $45.6 billion of U.S. health-care spending in 2008 to defensive medicine by physicians who ordered tests and procedures to protect themselves from malpractice suits.18
Does more screening mean better health outcomes?
The U.S. spends far more than other OECD countries on expensive diagnostic tests, but is the increased number of MRI and CT exams worth the cost? Using this equipment, doctors are capable of examining tissues in the human body and diagnosing a range of conditions. There is no question that MRI exams can save lives through early detection and treatment. Nonetheless, overuse is a concern. Not only are MRI exams expensive, they may register false positives and can lead to unnecessary treatments. Researchers at Stanford Medical Center found that areas in the U.S. with a high concentration of MRI machines had a higher number of patients undergoing MRI scans for lower back pain and, as a result, a higher number of people undergoing back surgeries. Many of these surgeries are deemed unnecessary by researchers in the scientific community, as most back pain tends to resolve itself over time. The study found that each additional MRI machine in a given area leads to 40 additional MRI scans, and that 3,500 unnecessary back surgeries could have been prevented if MRI equipment were unavailable.19
The high rate of screening in the U.S. may be more helpful in the diagnosis and treatment of two common cancers: breast cancer and colon cancer. The U.S. has the highest share of mammograph equipment per capita among its peers. Unfortunately, comparable mammography screening data are not available for the peer countries, but it is likely that the U.S. is a leader on this front given the relationship between equipment availability and usage. At 20.7 deaths per million population, the U.S. breast cancer mortality rate is much lower than that of many of its peer countries. Countries like Denmark, Ireland, and the U.K., which have a lower ratio of mammographs per population, have higher breast cancer mortality rates (29.5, 28.4 and 25.8 deaths per million population, respectively). Canada’s breast cancer mortality rate is slightly higher than that of the U.S.—22.4 deaths per million population in 2004—and it has a lower concentration of mammograph equipment: 21.3 per million population in Canada (2005) versus 40.1 in the U.S. (2008). The U.S. five-year relative survival rate for breast cancer is much higher than the OECD average as well.20
However, physicians are divided on the benefit of mammographies (also known as mammograms) for breast cancer screening. Many believe that better treatment, rather than more screening, is responsible for lower breast cancer mortality rates. A recently published Norwegian study suggests that increased awareness and improved treatment, not mammograms, are primarily responsible for reducing breast cancer mortality rates. According to the study, mammograms combined with treatment reduced the mortality rate for a test group by 10 per cent. But only one-third of the total estimated reduction in mortality was attributed to screening alone.21
The U.S. is a leader among its peers when it comes to the five-year survival rate for colon cancer, ranking second only to Japan.22 The colon cancer mortality rate in the U.S. is low compared with that of its peers. However, this may be more an indication of better treatment than increased screening. Colonoscopies—procedures that can not only detect precancerous growths but remove them as well—and other screening methods for colon cancer are being underused in the United States. According to results from the National Health Interview Survey, in 2005, “only 50 per cent of adults 50 or older had undergone a sigmoidoscopy23 or colonoscopy within the previous 10 years or had used a fecal occult blood home test kit within the preceding year.”24
Granted, screening rates may be even lower in other countries, which might be another explanation for the low colon cancer mortality rate in the U.S. relative to its peers. For example, in 2008, only 40 per cent of Canadians aged 50 and older reported that they had had up-to-date colon cancer testing.25 According to the U.S. Centers for Disease Control and Prevention, almost 60 per cent of colon cancer deaths could be prevented if those aged 50 and above had regular screening.26
Are higher prices another reason for higher health-care expenditures in the U.S.?
U.S. health prices were 25 per cent higher than the OECD average in 2005, according to the OECD. Prices in the U.S. are higher across the board. U.S. general practitioners, specialists, and nurses are paid significantly more than in other countries. Hospital services cost nearly twice as much as the average in 12 other OECD countries. And, U.S. pharmaceutical prices are anywhere between 30 and 50 per cent higher than the OECD average.27 Interestingly, health prices in Japan, the lowest health spender, were 25 per cent below the average in other OECD countries.
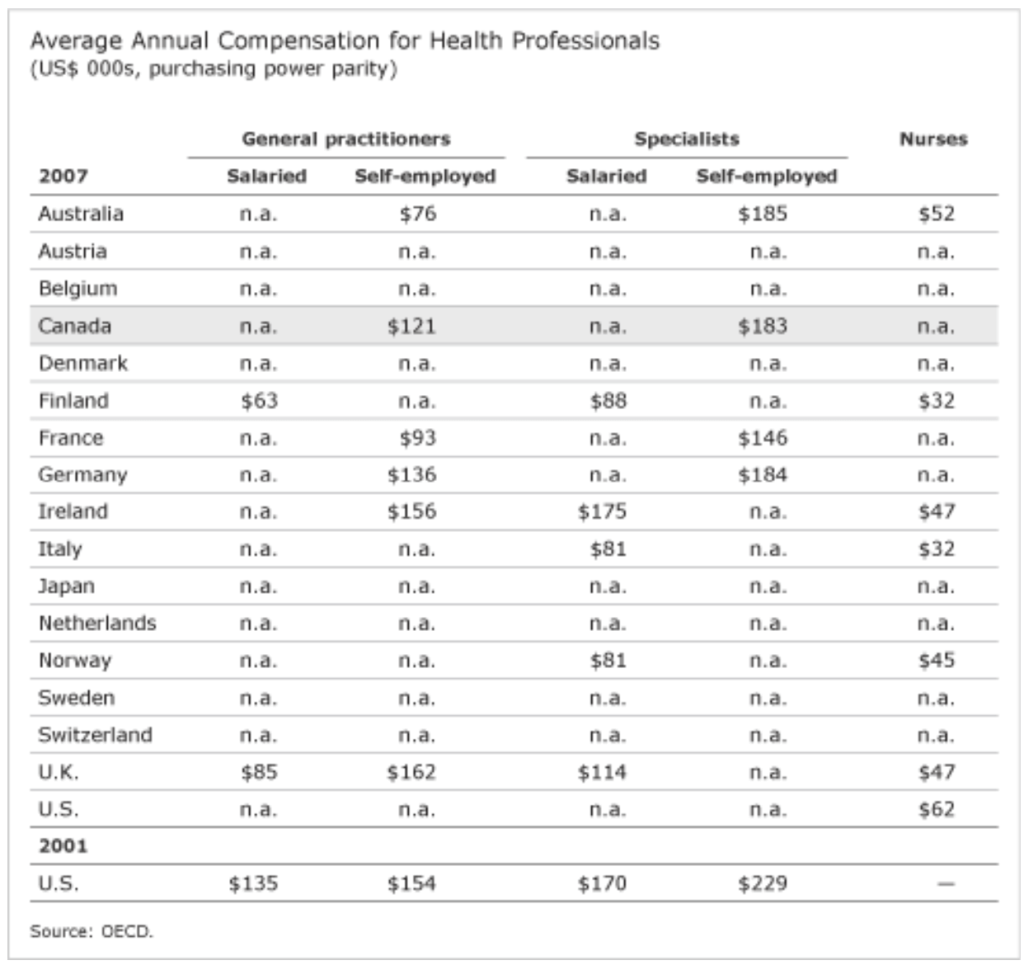
General practitioners (GPs) and specialists in the U.S. make significantly more than physicians in many of its peer countries. The latest available comparable U.S. data on physicians’ compensation are from 2001. In 2001, GPs in the U.S. made more than what GPs in most peer countries made in 2007. If up-to-date data were available for all countries, it would likely confirm that the U.S. has the highest-paid general practitioners. The same assessment applies to specialists’ salaries. Most peer countries’ specialists made less in 2007 than U.S. specialists earned in 2001.
More recent data are available for U.S. nurses. In 2007, nurses in the U.S. made $62,000 per year on average—$10,000 more than in Australia, where nurses have the second highest salaries among the peer countries.
While physicians in the U.S. are among the highest paid, they are also most likely to have the highest insurance premiums. Insurance costs for medical professionals are high for two main reasons: the high dollar amount of claims in the U.S. and the reduced supply of coverage.28 Also, malpractice litigation U.S. has high overhead costs. According to a U.S. study, “for every dollar spent on compensation, $0.54 went to administrative expenses (including those involving lawyers, experts and courts).”29 The high cost of medical liability insurance and the high dollar value of claims in the U.S. also encourage U.S. physicians to practise defensive medicine. The additional tests and procedures performed to protect physicians from the possibility of future lawsuits further exacerbates the problem of exorbitant health-care spending in the country.
What role does lifestyle play in rising health expenditures?
Why is it that with all its health-care spending, the U.S. performs poorly on broad measures of health such as life expectancy and potential years of life lost?
Obviously, health care is only one factor that affects health outcomes, albeit a major factor. Many factors outside the health-care system impact a country’s life expectancy and the loss of potential years of life. For example, crime and poverty affect the health of a population. On social indicators such as homicide and assault rates, as well as poverty rates, the U.S. ranks either last or very close to last in the comparator group.
Lifestyle factors such as tobacco consumption, poor eating habits, and inactivity affect health outcomes and increase health expenditures. Obesity may be a key reason why U.S. health spending is high and continues to rise. A study published by the journal Health Affairs indicates that medical spending for an obese person is $1,400 more per year, or 42 per cent higher, on average than for a normal weight person.30 Overall, obesity-related health-care spending is double what it was nearly a decade ago.
Obesity in the U.S. is reaching epidemic proportions and is increasing the prevalence of chronic conditions such as heart disease, hypertension, and Type 2 diabetes. All of these conditions are costly to the health-care system. Coronary bypass surgeries, angioplasties, and other cardiac surgeries are expensive procedures used to treat heart disease. In 2006, 84.5 coronary bypass surgeries per 100,000 population and 368.5 cardiac catheterization procedures per 100,000 population were performed in the United States. The U.S. has the highest mortality rate from Type 2 diabetes among the peer countries. The U.S. also has the highest hospital admission rates due to complications from diabetes—57 per 100,000 population in the U.S. versus the OECD average of 21. Medications used to treat chronic conditions related to being obese or overweight are also costly. Medicare spends about $600 more per year on prescriptions for an obese person than for someone of normal weight.31
So, lifestyle may be a huge reason why Japan has much better health outcomes than the United States, despite its much lower spending on health care. Less than 4 per cent of the Japanese population is obese. This is in stark contrast to the U.S., where one-third of the population is obese and nearly 70 per cent of the population is either overweight or obese. Tackling the obesity epidemic would be one way to address poor U.S. health outcomes and high health expenditures.
Use the bubble diagram to see the relationship over time between health expenditures and health outcomes, as well as the share of health resources, immunizations, surgical procedures performed, and diagnostics exams performed for the peer countries. Follow these steps:
- Under “Color,” choose “Country.” That way, each colour will represent a specific country. (When you scroll over each different coloured bubble, the country name will pop up.)
- Under “Size,” we recommend you choose “Population” or “GDP per capita” as the variable that determines the size of the bubble. That way, you will be able to see at a glance how bigger countries are doing compared with smaller ones, or how richer countries are doing compared with poorer ones.
- Choose a health expenditure variable such as “Health spending (% of GDP)” to track on the horizontal axis.
- Choose a health outcome such as “Life expectancy” as the variable to track on the vertical axis.
- If you want to see a trail for a particular country, click in the “Trails” box, and then click in the box of the country (or countries) you want to trail. Each country will be represented by a trail of bubbles in its unique colour.
- Finally, click the play button in the bottom left to begin the show.
Footnotes
1 Canadian Institute for Health Information, National Health Expenditures Database (NHEX).
2 OECD Health Data 2010. Dollar amounts are in U.S. dollars, purchasing power parity. Purchasing power parity (PPP) converts income more accurately across countries than using nominal exchange rates. The purchasing power parity rate is set so that a fixed basket of goods and services in one country will have the same value if expressed in the currency of another country.
3 Data for 2008 health expenditure per capita for Canada, Denmark, and Finland. 2007 data for Australia.
4 Data for 2008 are not available for the following peer countries: Australia, Denmark, Japan, Ireland, Switzerland, and the United Kingdom. Data for 2008 on inpatient and outpatient care expenditures are not available for the Netherlands.
5 Cathy Schoen, Robin Osbourn, Michelle M. Doty, David Squires, Jordon Peugh, and Sandra Applebaum, A Survey of Primary Care Physicians in Eleven Countries, 2009 (The Commonwealth Fund, November 2009), 4.
6 Barbara Starfield, Leiyu Shi, and James Macinto, Primary Care Contributions to Health Systems and Health, 2005 (Baltimore: The John Hopkins School of Public Health), 18.
7 McKinsey Global Institute, Accounting for the Cost of U.S. Health Care: A New Look at Why Americans Spend More (McKinsey & Company, December 2008), 43.
8 Ibid., 51.
9 Ibid., 45.
10 Based on 2008 data. In 2007, both Switzerland and Norway had higher inpatient expenditures per capita than the U.S. 2008 data are not available for Switzerland.
11 OECD 2010 Health Data.
12 Mark Pearson, “Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend So Much More Than Other Countries?” Written Statement to Senate Special Committee on Aging, September 2009, 9.
13 The Conference Board of Canada, Liability Risks in Interdisciplinary Care: Thinking Outside the Box (Ottawa: CBoC, April 2007), 35.
14 Note: The average includes 12 countries. Data are not available for the following countries: Canada, France, Ireland, Italy, and the Netherlands.
15 NPR, “In Japan, MRIs Cost Less,” All Things Considered, November 18, 2009.
16 Mark Pearson, “Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend So Much More Than Other Countries?” Written Statement to the Senate Special Committee on Aging, September 2009, 9. Note: Data for Japan are not available and were not used in calculating the OECD average.
17 Defensive medicine is the delivery of medical services primarily to minimize physicians’ liability risks.
18 Michelle M. Mello, Amitabh Chandra, Atul A. Gawande, and David M. Studdert, “National Costs of the Medical Liability System,” Health Affairs, 29, 9 (September 2010), 1570.
19 Dotmed News, (accessed February 4, 2011).
20 Mark Pearson, “Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend So Much More Than Other Countries?” Written Statement to the Senate Special Committee on Aging, September 2009, 9.
21 Mette Kalager and Marvin Zelen, “Effect of Screening Mammography on Breast Cancer Mortality in Norway,” The New England Journal of Medicine (September 23, 2010), 1206–1207.
22 Mark Pearson, “Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend So Much More Than Other Countries?” Written Statement to the Senate Special Committee on Aging, September 2009, 9.
23 A sigmoidoscopy is a screening test in which the physician examines the lining of the rectum and lower portion of the colon using an instrument with a small built-in camera. A fecal occult blood test is a test that checks for hidden blood in the stool.
24 Centers for Disease Control and Prevention, “Colorectal Cancer Screening Rates” (accessed September 23, 2010).
25 Up-to-date colorectal cancer testing is defined by Statistics Canada as having a fecal occult blood test in the past two years, or sigmoidoscopy or colonoscopy in the past five years. Statistics Canada, Study: Mammography Use and Colorectal Cancer Testing.
26 Centers for Disease Control and Prevention, “Colorectal Cancer Screening Rates.”
27 Mark Pearson, “Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend So Much More Than Other Countries?” Written Statement to the Senate Special Committee on Aging, September 2009, 7–8.
28 The Conference Board of Canada, Liability Risks in Interdisciplinary Care: Thinking Outside the Box (Ottawa: CBoC, April 2007), 35.
29 Ibid.
30 Eric A. Finkelstein, Justin G. Trogdon, Joel W. Cohen, and William Dietz, “Annual Medical Spending Attributable to Obesity: Payer- and Service-Specific Estimates,” Health Affairs, 28, 5 (July 27, 2009), w828.
31 Ibid., w828.